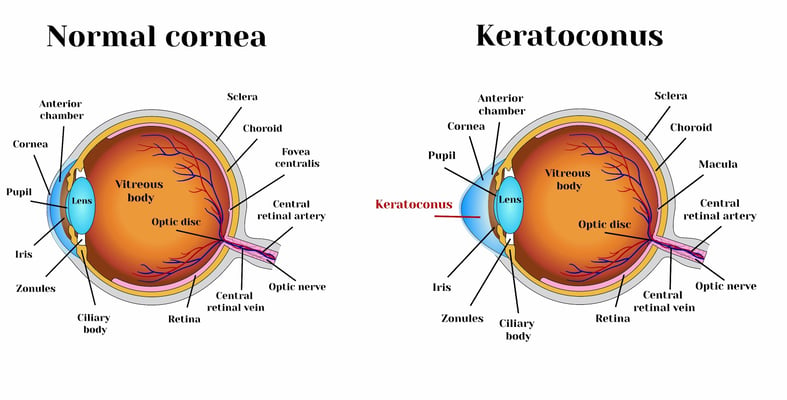
Keratoconus and cataracts , symptoms and types

Basal metabolic rate
It is the number of calories the body burns while performing its basic functions to sustain life.

BMI index
It is a semi-accurate indicator of body fat percentage and obesity.

Water calculator
This calculator helps you calculate the amount of water you need to drink to maintain body functions and avoid dehydration

calorie calculator
This calculator estimates how many daily calories your body needs to maintain your current weight
Treatment Services
In the Best Medical Centers
Contact Us
Please fill the form below and describe your condition, We will contact you back
Select Service
- Dental Treatment
- Hair Transplant
- Obesity Surgery
- Vision Correction
- Health Resorts
- Other Medical Services
- No elements found. Consider changing the search query.
- List is empty.
Your personal data is processed as indicated in the general statement text and by continuing, you explicitly consent to the processing

